I (Leigh) have had a front row seat to the challenges of rheumatoid arthritis (RA) for the past ~20 years. I’ve watched both my mom and my aunt develop and manage this disease. I’ve watched them navigate the maze of diagnostic tests, decipher confusing lab results, cycle through multiple treatments to find what actually works, and then- perhaps the hardest part- advocate for themselves with insurance companies to get those (often very expensive) therapies covered.
Because of that history, I know RA may one day be part of my own story too. I’ve already had blood tests for RA-associated markers (so far, so good!), but I stay vigilant. Any joint issue I have gets checked out, and every clinician I see knows my family history. I’m a big believer in the power of awareness and early screening to make all the difference in long-term health and quality of life.
This might sound bleak and depressing, but there’s also good news. The RA landscape today looks very different from when my mom and aunt were first diagnosed. And working as a scientist in drug development, I’ve had a front-row seat to these changes. Diagnostics are more specific, treatment options are broader and more personalized, and there’s an exciting pipeline of new therapies on the way. That progress gives me, and a lot of other families, real hope: RA might impact quality of life, but it doesn’t have to derail it.
Even today, I can see my mom enjoying her retirement, gardening and playing with her grandchildren, thanks to the development of drugs like Enbrel (etanercept) and Rinvoq (upadacitinib), and the added utility of corticosteroids (prednisone). Full disclosure: I don’t work in pharma, and neither my mom nor I receive any financial compensation for mentioning these drugs. I’m just grateful that her flares are under control and that she can enjoy playing with my kids!
What is Rheumatoid Arthritis?
Rheumatoid arthritis is a chronic autoimmune disease that affects millions of people worldwide—about 208 out of 100,000 people. In this condition, the immune system makes a serious mistake: it attacks the joint lining (synovium), leading to inflammation, pain, and progressive joint damage. It primarily affects joints in the hands, wrists, and feet, but it doesn’t always stop there. It can also involve the eyes, lungs, heart, skin, and blood vessels.
The word ‘arthritis’ literally means inflammation of a joint, but it’s not just one disease. It’s an umbrella term for many different conditions that can look very different from each other. You might have heard of osteoarthritis (OA). That’s the “wear and tear” arthritis that comes from years of use. It occurs when cartilage gradually wears down over time and is not considered an autoimmune disease. RA, on the other hand, is driven by immune system dysfunction and inflammation that actively damages the synovium. Because of this fundamental difference, RA may begin earlier in life, progress differently, and require specialized treatments that target the immune system itself.
What makes RA particularly tricky? Symptoms can look like other conditions and vary widely from person to person, making it challenging to understand and sometimes difficult to diagnose.
Let’s take a closer look at what may play a role in RA development, common signs and symptoms, and how it can be treated.
When the immune system mistakenly identifies joints as intruders
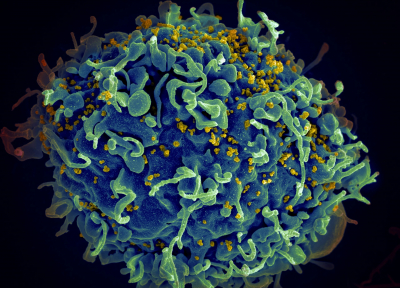
Imagine your immune system as a security guard. In rheumatoid arthritis, this guard starts seeing your own joints as threats—attacking them with the same force it would use against actual invaders. But what flips that switch from protector to attacker?
The answer, frustratingly, is: it’s complicated. Like many autoimmune conditions, RA is a complex disease driven by multiple factors. The exact cause is unknown, but several specific factors can create the perfect storm for its development. These include genetic susceptibility, environmental influences, hormonal factors, and immune dysregulation. Together, these elements contribute to the loss of immune tolerance and the chronic inflammation that characterizes the disease:
- Genetics: A family history of RA increases risk, which is why I keep such close tabs on my own joint health. Variants of genes involved in immune regulation are strongly associated with RA, but genetics alone does not cause the disease. One example is HLA-DRB1, which encodes a protein that presents peptide antigens to T cells (essentially showing the immune system what to target). Having certain variants of this gene is associated with an increased risk of RA. You can think of it as having a genetic “vulnerability”- the door is there, but something still needs to open it.
- Environmental Factors: Certain exposures can trigger disease in genetically predisposed people, including:
- Cigarette smoking
- Air pollution
- Occupational dust (like silica)
- Hormonal influences: As with several autoimmune conditions, RA is 2-4 times more common in women than in men (my mom and her sister both have it but their brother does not). Peak onset tends to occur during times of hormonal flux, such as the postpartum period and perimenopause. This isn’t a coincidence; hormones play a significant role in immune regulation.
- Health influences: Poor dental health and the persistent presence of certain microorganisms, such as Porphyromonas gingivalis (a bacterium associated with gum disease), may be associated with the development of RA.
What RA looks and feels like
RA is particularly sneaky because the underlying immunological changes that cause it can begin years before the disease becomes symptomatic. The immune system may be quietly turning against the joints long before a person feels anything wrong.
When symptoms finally do show up, they can develop gradually and become progressive, worsening over time. The disease can also ebb and flow with cycles of flares (periods of intense symptoms) and remission (when symptoms subside).
One key distinguishing feature of RA is that the symptoms often affect the same joints on both sides of the body (like both wrists or both knees). This symmetry helps to distinguish it from osteoarthritis, which often affects only one side.
RA symptoms develop most frequently between the ages of 30 and 60.
- Pain, swelling, and stiffness in more than one joint (typically hands, wrists, or feet)
- Stiffness that is worse in the morning and lasts more than 30-60 minutes
- Warmth or tenderness in the joints
- Fatigue
- Weakness
Because RA is systemic and affects the entire body, other manifestations may occur:
- Eye inflammation (dry eyes, scleritis) and dry mouth
- Lung inflammation or scarring (up to 80% of people have lung involvement)
- Skin nodules or rashes
- Anemia
- Increased cardiovascular risk, such as atherosclerosis, heart attack, stroke, and pericarditis
- Loss of bone density from chronic inflammation
Symptoms vary widely from person to person, depending on the stage of the disease and other health conditions. No two RA stories look exactly the same.
Piecing Together a Diagnosis
There is no single blood test that says “yes, you definitely have RA.” Instead, diagnosing RA typically involves a combination of clinical evaluation, laboratory testing, and imaging studies. It’s like putting together a puzzle where each piece adds clarity.
The diagnosis is often made or confirmed by a rheumatologist after a patient is referred by their primary care physician or another clinician who suspects RA. Since RA is systemic and can affect multiple organ systems, a person with RA can end up working with a whole team:
- Rheumatologists, who specialize in the diagnosis and care of autoimmune and connective tissue diseases
- Dermatologists, for skin manifestations like rashes and lesions
- Hematologists, to address blood-related complications
- Cardiologists and pulmonologists, when the heart or lungs are involved
- Ophthalmologists, when eye complications occur
- Orthopedists, when bones are impacted negatively
- Endocrinologists, for hormonal issues
Blood tests detect inflammation and autoantibodies (antibodies that mistakenly attack the body’s own tissues):
- Rheumatoid Factor (RF) – These autoantibodies are present in the blood of many RA patients, though not specific to the disease (that is, you can have RF in the blood and not have RA, or you can have RA and not have RF in the blood).
- Anti-Citrullinated Peptide Antibody (ACPA) – These autoantibodies are highly specific for RA and may predict severity (this is the one my mom tests positive for).
- Erythrocyte Sedimentation Rate (ESR) – An elevated sedimentation rate in red blood cells (erythrocytes) is a non-specific marker of inflammation.
- C-reactive protein (CRP) – Elevated levels of CRP in the blood indicate inflammation.
- Complete Blood Count (CBC) – This measures amounts and sizes of red blood cells, white blood cells, platelets, and hemoglobin to evaluate for anemia or other blood abnormalities.
Imaging evaluates joint damage and inflammation. Early in the disease, imaging may appear normal, but inflammation can progress silently. This is why early detection is so important. Imaging options include X-ray, ultrasound, and magnetic resonance imaging (MRI).
Clinical evaluation: A physician will examine your joints to determine how many are involved and where, ask about the duration of pain and stiffness, and evaluate swelling. This hands-on assessment, combined with diagnostic testing, is essential for diagnosing the disease.
Diagnosis of RA is guided by ACR/EULAR classification criteria, which incorporate symptoms, antibody tests, and inflammation markers. Early referral to a rheumatologist is recommended when RA is suspected.
It is also important to note that there are multiple varieties of rheumatoid arthritis, including seronegative forms which can be negative for RF, ACPA, or both. My mom is seronegative for RF but seropositive for ACPA- proof that human bodies don’t always read the textbook.
How RA is treated
While there is no cure for RA, treatments can reduce symptom severity, prevent joint damage, and improve quality of life. Without her RA treatments, my mom wouldn’t be able to enjoy her retirement gardening and playing with her grandchildren.
Treatments focus on controlling inflammation and stopping disease progression. Here’s what’s available:
Disease-Modifying Antirheumatic Drugs (DMARDs): These medications alter immune activity to prevent joint destruction. They work by modulating immune cell function and reducing inflammatory signaling and, ultimately, inflammation. Options include methotrexate (the most common first-line therapy), sulfasalazine, leflunomide, and hydroxychloroquine (yes – the antimalarial drug, but it works by a different mechanism here).
Targeted DMARDs: Small-molecule inhibitors taken orally, such as JAK inhibitors (tofacitinib, baricitinib, upadacitinib). These block intracellular inflammatory signaling pathways, essentially turning down the volume on inflammation.
Biologic Therapies: Engineered antibodies or receptor molecules that target specific immune pathways involved in RA development and progression. These are large protein molecules given by injection or infusion (they can’t be absorbed if taken orally). Examples include:
- TNF inhibitors (etanercept, adalimumab, infliximab) target and block tumor necrosis factor (TNF), a pro-inflammatory cytokine. When TNF can’t bind to receptors on immune cells (like macrophages), the inflammatory cascade is prevented.
- IL-6 inhibitors target and block interleukin-6 (IL-6), another pro-inflammatory cytokine. This decreases T and B cell activation.
- B-cell depleting antibodies (rituximab) target and eliminate B cells to reduce the production of autoantibodies. This is a well-established option for patients who do not respond well to TNF inhibitors.
- T-cell co-stimulation blockers target the co-stimulatory protein CD28 on T cells to block activation.
Corticosteroids: Corticosteroids like prednisone and methylprednisolone rapidly reduce inflammation during flares. These immune-suppressing medications form complexes with cellular proteins that travel to the nucleus and suppress inflammatory gene expression.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): For mild symptoms, medications like ibuprofen, naproxen, and meloxicam help reduce inflammation and control pain by inhibiting COX enzymes involved in inflammation.
Innovative treatments: Several new treatments are in development for RA:
- Next-generation JAK inhibitors with fewer side effects and improved specificity
- Novel cytokine blockers (like the IL-6 treatment mentioned above)
- BTK inhibitors, which target B cell signaling (already approved for some cancers, now being tested for RA)
- Immune checkpoint blockade to block immune activation
- CAR-T therapy and gene editing of HLA genes
- Medical devices like vagus nerve stimulation devices
- Diagnostic tools like rapid synovial fluid biomarker analysis, which can help distinguish RA from osteoarthritis with robust biomarkers in about 10 minutes!
Some advances are still in preclinical stages, while others have entered clinical trials. The pace of innovation is truly exciting!
Final Thoughts
Rheumatoid arthritis is one of the most common autoimmune conditions, and it affects far more than joints. It’s shaped by genetics, environment, hormones, and health factors that vary widely from person to person. No two RA stories look exactly the same.
But advances in rheumatology and drug development have transformed RA from a highly disabling disease into one that can often be managed effectively with early treatment. My mom is proof. She’s gardening, chasing grandkids, and living her retirement, not defined by her diagnosis. A healthy lifestyle, including regular exercise and a balanced diet, can provide additional support in managing the disease.
If you’re living with RA, you’re not alone. And if you’re like me, watching and waiting, knowledge is power. Early detection matters. So does having a team you trust.
Resources for Support
If you or someone you care about has been diagnosed with RA—or you suspect RA might be a concern—we’ve gathered a list of trusted resources to help you learn more and find support.
- https://www.ra.com/rheumatoid-arthritis-resources/ra-support
- https://www.arthritis.org/rheumatoid-arthritis-patient-education
- https://rheumatology.org/living-with-rheumatoid-arthritis
- https://rheumatology.org/patients/rheumatoid-arthritis
This article is a collaboration with Unbiased Science, an organization of multidisciplinary scientists dedicated to making health and science information accessible to the public and meeting people where they are.