Imagine thinking you’ve recovered from COVID, only to find yourself grappling with persistent and often debilitating symptoms for weeks, months, or even years. Shockingly, around 30% of adults in the U.S. who’ve battled COVID reported experiencing long COVID. What’s even more surprising is that the majority of them started with just a mild case of the virus.
If you’re seeking information, know you aren’t alone. Here’s what the scientific community understands about long COVID — its causes and symptoms, who is at risk, and the questions we’re still working to answer.
What exactly is long COVID?
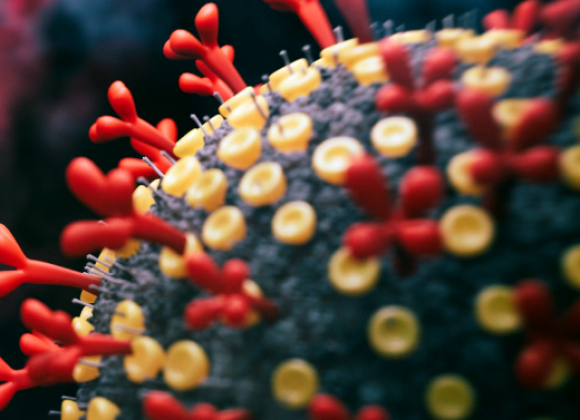
Long COVID is a set of chronic illnesses triggered by infection with SARS-CoV-2, with symptoms that typically start within the first three months of getting COVID and last at least for more than four weeks or two months. Long COVID itself can last for months or even years. Women and people in their 30’s to 60’s are at a higher risk of developing long COVID. We are still lacking reliable diagnostic tools and there are no effective therapies for long COVID. Long COVID likely consists of multiple diseases.
What causes long COVID?
While we do not know exactly what causes long COVID, there are four key hypotheses that we suspect are the root causes. Over the past four years, many studies have supported the existence of these possible disease drivers:
- Viral persistence – Viral pieces (RNA and proteins) have been found in many organs from some people who had COVID months to years before. Replicating virus may be present.
- Autoimmunity – Autoantibodies are found in a subset of long COVID patients.
- Chronic changes in immune cells – Chronic changes in the immune cells in the brain have been noted in both animal models and some patients.
- Reactivation of latent herpesviruses – Some patients have signs of reactivation of dormant herpes viruses such as Epstein-Barr Virus.
The ultimate proof will come from clinical trials that target the root causes.
Why do some people get long COVID and not others?
We still don’t have a complete answer to this question. The severity of acute infection will increase the likelihood of long COVID outcomes, as well as certain variants of concern. Factors such as middle age, sex hormones, and the X-chromosome and its inactivation process likely contribute to the heightened risk for women. Our work found that lower levels of testosterone are a top predictor of long COVID status in females. There may also be genetic risks associated with long COVID, but more studies are needed to map out the susceptibility genes.
How does long COVID affect the immune system?
Long COVID can impact the immune system in multiple ways.
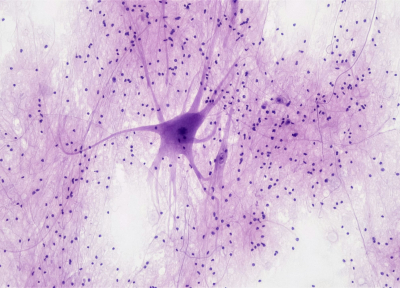
- Neurological Impact
In a mouse model of mild respiratory COVID, immune cells in the brain called microglia become activated, chronically damaging the surrounding supportive cells and ultimately neurons. These changes could explain neurocognitive deficits. - Antibody and Autoantibody Production
Antibodies to the spike protein, the major target of immune attack, become elevated. Autoantibodies are produced in some patients, that may attack and damage various organs leading to autoimmunity. - T Cell Skewing
Spontaneous interferon-gamma secretion from T cells is seen in patients. Type 2 immune responses are detected in T cells in the blood after stimulation. Virus-reactive T cells show signs of exhaustion, suggestive of the inability of the body to remove SARS-CoV-2. - Herpes Virus Reactivation
Reactivation of Epstein-Barr virus, especially in women. - Systemic Impact
In addition to the immune system, long COVID appears to impact the nervous system and the endocrine system, leading to lower levels of cortisol.
Is it possible to prevent long COVID?
The best way to prevent long COVID is to avoid getting COVID in the first place. Being up to date with the vaccine and booster doses, masking in crowded indoor settings, enhancing ventilation, rapid testing before gathering, and paying attention to the viral levels in the community through wastewater surveillance are all good ways to achieve this goal.
However, no matter how careful, it is not possible to avoid the virus altogether. Once you get COVID, it is important to take enough time to rest and recover, to reduce the chances of developing complications including long COVID. Getting antivirals to treat the acute infection might help prevent long COVID, especially if you are in a high-risk group.
What does the future of long COVID therapy look like?
While we do not yet have effective therapies to treat long COVID, multiple clinical trials are being conducted to get at the root of the problem. Antivirals and monoclonal antibodies may treat persistent SARS-CoV-2 virus. Autoimmunity can be treated with existing medicine. Chronic inflammation can be treated with immune modulators. Reactivated herpes viruses can be treated with antivirals. In addition to repurposing existing therapies, new drugs may be developed to combat these disease drivers. Identifying biomarkers of success can translate to targeted and effective treatment for patients with long COVID in the future.