How the immune system fights cancer
Learn how the immune system protects you from developing cancer and how cancer cells adapt to hide from it.
On This Page:
Overview
Your immune system is your body’s defense mechanism that helps to keep you healthy. It’s designed to protect you from infections, harmful substances, and even cancer. Every day, it patrols your body for anything that shouldn’t be there, including cancer cells.
When everything is working as it should, the immune system can spot when one of your own cells is behaving abnormally, like growing too fast, dividing when it shouldn’t, or carrying damaged DNA. These are all hallmarks of a cancer cell.
Understanding how the immune system helps protect against cancer can give us powerful insights into how cancer develops and how we can treat it.
Key Points
- The immune system constantly monitors the body and can detect and destroy cells that may become cancerous.
- Cancer can develop when it evades or suppresses the immune system’s natural defenses.
- Immunotherapies help the immune system fight cancer by boosting, reactivating, or enhancing immune responses.
How the Immune System Detects and Destroys Cancer Cells
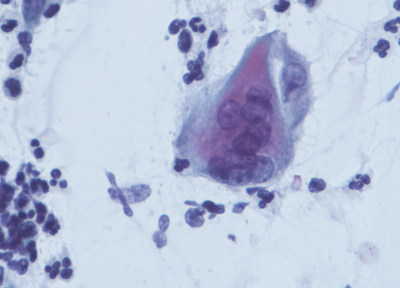
Cancer starts when cells in the body grow out of control. Normally, the immune system can detect these early changes because cancer cells often look different on the surface. They may produce unusual proteins or signals that alert immune cells to their presence. Immune cells, such as T cells and natural killer cells, spring into action to hunt down and destroy any abnormal cancer cells.
In many cases, this process happens without us ever knowing. Your immune system might stop cancer before it even has a chance to grow.
How Cancer Cells Hide from the Immune System
Unfortunately, cancer can be tricky. Some cancer cells learn how to hide from the immune system or turn off immune responses. Examples of how cancer cells can hide from the immune system include:
- Camouflage – Some cancer cells stop showing the “danger” signals that normally alert immune cells
- Immune suppression – Cancer cells that make up a tumor can release chemicals that weaken or block immune cell activity in their area.
- Altering the environment – Cancer cells can change the physical and chemical environment around them, making it difficult for immune cells to infiltrate the tumor or function effectively.
- Exhaustion – Over time, constant battle with a growing tumor can wear out immune cells, making them less effective.
When cancer cells are successful at hiding, they can grow and spread without being stopped.
What Does This Mean for Cancer Treatment
Understanding how the immune system fights cancer, and what goes wrong, has led to one of the most exciting areas in cancer research: immunotherapy. These are treatments that help the immune system better recognize and destroy cancer cells.
The most common types of immunotherapies include:
- Checkpoint Inhibitors – Some cancers produce proteins that act like “brakes” on immune cells, stopping them from attacking. Checkpoint inhibitors are drugs that release these brakes, allowing T cells to do their job.
- CAR T Cell Therapy – This is a highly personalized treatment where a patient’s own T cells are collected, genetically modified in a lab to better recognize cancer, and then returned to the body.
- Cancer Vaccines – Cancer vaccines don’t prevent cancer like traditional vaccines prevent infection, but instead help the immune system recognize and attack cancer cells.
Sources
- Jain, A., Marshall, J., Buikema, A., Bancroft, T., Kelly, J. P., & Newschaffer, C. J. (2015). Autism Occurrence by MMR Vaccine Status Among US Children With Older Siblings With and Without Autism. JAMA, 313(15), 1534. https://doi.org/10.1001/jama.2015.3077
- Taylor, B., Miller, E., Farrington, Cp., Petropoulos, M.-C., Favot-Mayaud, I., Li, J., & Waight, P. A. (1999). Autism and measles, mumps, and rubella vaccine: no epidemiological evidence for a causal association. The Lancet, 353(9169), 2026–2029. https://doi.org/10.1016/s0140-6736(99)01239-8
- Madsen, K. M., Hviid, A., Vestergaard, M., Schendel, D., Wohlfahrt, J., Thorsen, P., Olsen, J., & Melbye, M. (2002). A Population-Based Study of Measles, Mumps, and Rubella Vaccination and Autism. New England Journal of Medicine, 347(19), 1477–1482. https://doi.org/10.1056/nejmoa021134
Related Topics
Downloads
External Resources
Latest News