For decades, biology textbooks described the nervous system and immune system as operating in separate worlds: one governing thoughts and sensations, the other defending against infections. But we now know that’s not exactly the case. The immune and nervous systems are in constant conversation, forming an integrated network that keeps the body balanced.
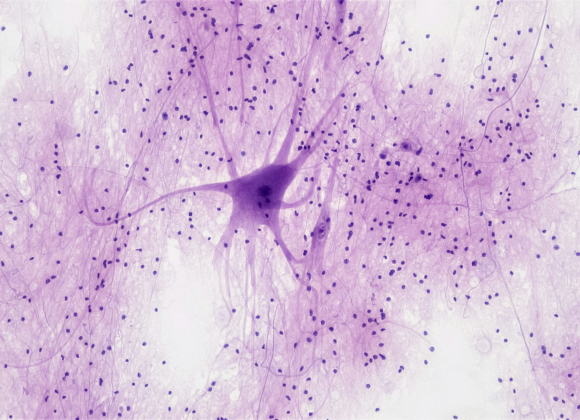
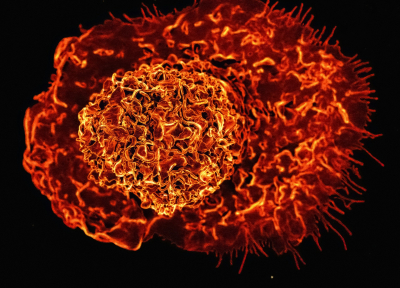
The field of neuroimmunology aims to decode these conversations between glia (nervous system cells) and lymphocytes (immune cells) and understand what happens when that communication goes awry. T cells, microglia, astrocytes, macrophages, dendritic cells, and many more – these cells form a kaleidoscopic community that adapts and responds to the body’s every experience.
The brain’s immune connections extend into nearly every corner of physiology and behavior. Immune signals ebb and flow with the body’s natural timekeeping system known as the circadian clock helping the body anticipate the recurring environmental changes over a 24-hour cycle. Crucially, immune cells have their own internal clocks but are all linked to the master clock that lives in hypothalamus region of the brain.
Immune cells can also influence the flow of cerebrospinal fluid (CSF) which is the liquid that bathes the brain and spinal cord shaping how nutrients and waste are exchanged in the nervous system. Immune activity can even alter behavior during illness. In fact, research shows that inflammation can drive social withdrawal. This adaptive strategy separates sick individuals away from the healthy helping to limit the spread of the infection.
Multiple Sclerosis
This growing understanding is already reshaping medicine. Therapies once thought of as purely neurological, such as those for multiple sclerosis (MS) or Alzheimer’s disease, are increasingly being viewed through an immunological lens. At the same time, immune-targeting drugs are being re-examined for their effects on mood, cognition, and neurodegeneration. Nowhere is this shift clearer than in MS, which offers a powerful example of neuroimmune interactions gone wrong.
In MS, the immune system mistakenly attacks the myelin sheath, which is the protective insulation surrounding nerve fibers in the brain and spinal cord. A helpful analogy is thinking of our nerves as cables, with myelin as the plastic insulating coating that allows signals to travel more efficiently. When that coating is stripped away, signals can still pass, but they’re slower, weaker, and sometimes lost altogether. This loss of myelin (demyelination) arises from immune cells breaching the nervous system’s barriers, sparking inflammation that further disrupts communication between neurons. The result is a wide range of neurological symptoms including most commonly: fatigue, numbness, vision loss, and difficulty moving. These wide-ranging symptoms clearly reflect this breakdown in the brain-immune dialogue.
Unlocking New Therapies
While we still don’t fully understand the exact sequence of events that drive MS progression, our growing insight into the immune mechanisms involved has already revolutionized treatment. Over the past 25 years, more than a dozen new therapies have been approved, most of which target immune pathways to calm inflammation, block lymphocyte entry into the brain, or modulate immune signaling. Many of today’s most effective MS drugs work not by repairing the myelin, or coating, of the neurons directly, but by restoring balance to the immune system itself allowing the body’s natural repair mechanisms to kick in. Yet even as MS remains the flagship example, it’s becoming clear that immune–nervous system interactions reach far beyond this one disease.
The more we uncover about the dialogue between the immune and nervous systems, the clearer it becomes that health is not the absence of disease but the balance of connection. What began as two separate disciplines has become a shared language; an ongoing conversation of signals, cells, and responses that shape how the body thinks and feels. Each discovery in neuroimmunology not only rewrites the textbooks but deepens our understanding of this exchange. The boundaries between the nervous and immune systems are dissolving, giving rise to a new kind of medicine.